Os Trigonum and Os Peroneum Syndrome – Extra Bones in Ankle or Foot
The os trigonum and os peroneum are accessory ossicles (extra bones) in the ankle/foot that are present at birth (congenital) in some people. Most of the time, these extra bones go unnoticed. They may be identified on x-rays, but are often asymptomatic and do not need to be addressed. However, as a result of overuse or an injury, these bones and the surrounding tissue and/or joints may become inflamed and painful. The terms Os Trigonum Syndrome and Os Peroneum Syndrome are used to describe the painful symptoms.
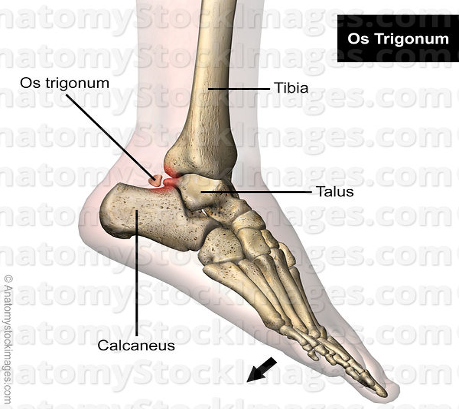
The os trigonum can form behind the ankle bone (talus) during adolescence when it does not fuse with the rest of the ankle bone leaving a small extra bone. This bone can get pinched between the talus and calcaneus (heel bone) with repeated downward pointing of the foot/toes during sports activity (eg – soccer). Ballet dancers can develop a “nutcracker injury” due to spending frequent and prolonged time on their toes which can crunch the os trigonum causing inflammation in the area.
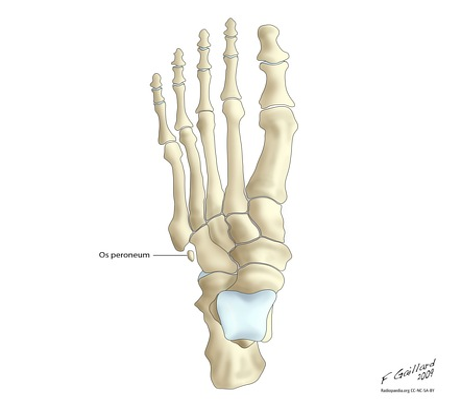
The os peroneum is an accessory bone that is located in the peroneus longus tendon which passes over the lateral aspect of the foot. About 1 in 5 people have this extra bone. This bone and the surrounding tendon can become inflamed with repetitive activity such as running and jumping or with an acute injury like an ankle sprain.
Signs and symptoms of both these syndromes include: swelling in the back of the ankle (os trigonum) or lateral foot (os peroneum), tenderness in the area, pain with pushing off the foot/toes when walking, and weakness. X-rays or other imaging can confirm the presence of these accessory bones.
Conservative treatment of these syndromes involve the following:
- Rest – avoiding aggravating activities such as running, jumping, dancing, etc.
- Immobilization – a walking boot may be prescribed to limited motion of the ankle/foot
- NSAIDs and cold packs – to reduce pain and inflammation
- Physical Therapy – to restore normal flexibility/mobility, increase strength/stability and assist with return to ADLs and recreation/sports
If symptoms persist, then steroid injections may be used. Surgical intervention may be required to remove the os trigonum or os peroneum. Following surgery, physical therapy can be prescribed to regain ROM, strength, balance/stability, endurance, and to facilitate return to prior level of function.
If you have questions or would like to learn more about this topic, contact the therapy professionals at ProActive Physical Therapy and Sports Medicine for help.
For Accessory Navicular Syndrome Exercises, Visit One of Our San Diego Area Clinics
Rancho Bernado Physical Therapy Clinic
Carlsbad Physical Therapy Clinic
Carmel Valley Physical Therapy Clinic
Mission Valley Physical Therapy Clinic




 What are common causes of neck pain?
What are common causes of neck pain?

 Both words are spelled correctly but tendinitis tends to be the more preferred term used in medical literature. More importantly, what is upper extremity tendinitis? The suffix “itis” means inflammation and the term tendinitis should be reserved for tendon injuries that involve larger-scale acute injuries accompanied by inflammation.(1) Risk factors include repetition, awkward postures, direct pressure, high force and prolonged static positioning.(2)
Both words are spelled correctly but tendinitis tends to be the more preferred term used in medical literature. More importantly, what is upper extremity tendinitis? The suffix “itis” means inflammation and the term tendinitis should be reserved for tendon injuries that involve larger-scale acute injuries accompanied by inflammation.(1) Risk factors include repetition, awkward postures, direct pressure, high force and prolonged static positioning.(2)
