Tendon injuries are among the most common injury types affecting the lower extremity, with involvement of the Achilles’ tendon being especially prevalent. Achilles’ pain can affect young and middle age athletes, as well as the less active and older individual. Achilles’ injuries vary in the type of tissue damage involved, and treatment of these injuries can vary dramatically, depending on the state of the tendon. Damage to the Achilles’ can vary from an acute inflammation (“tendinitis”), to a chronic degenerative state (“tendinosis” or “tendinopathy”), to complete tearing or rupture of the tendon. All three of these conditions generally involve a problem with loading of the tendon, yet each one demands a significantly different treatment approach.
Ruptures of the Achilles’ tendon involve complete tearing of the tendon, and are usually the result of a rapid, extreme loading of the tendon, commonly seen in sports such as tennis, basketball and soccer. Individuals typically describe a sensation of hearing a gunshot or car backfire, associated w/ pain and immediate disability. Treatment of a complete rupture generally involves surgical repair of the tendon, followed by brief immobilization and then gradual resumption of stretching and strengthening over the next several months under the supervision of a physical therapist. Reports on outcome following Achilles’ ruptures show a lower re-tear rate for those undergoing surgical repair versus those treated non-operatively.
Acute tendinitis can also result from overloading of the Achilles’ tendon, but these loads are lower and more repetitive in nature. Tendinitis is generally of recent onset (less than six weeks), and can often be traced to a change in loading of the tendon, such as increased duration, repetitions or distance of training (“training errors”). Treatment of acute tendinitis generally involves the “RICE” principle of rest, ice, compression and elevation. Examination for training errors, or any preexisting biomechanical issues (tight calf musculature, limited ankle mobility or faulty movement patterns) can help reduce risk of recurrence.
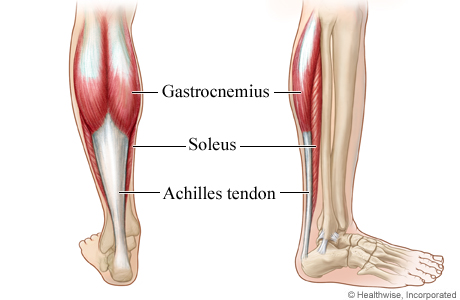
Tendinosis, or tendinopathy, is a condition in which acute inflammation is no longer present, and the tendon has undergone physiologic changes that negatively affect the ability for the tendon to heal or to normally attenuate load. Achilles’ tendinopathy is frequently categorized by the location of tissue damage and pain. “Insertional” tendinopathy occurs at the most inferior portion of the tendon, as it inserts into the heel bone (calcaneus), and typically affects a less-active, older population. “Non-insertional” tendinopathy usually involves tendon thickening and pain approximately 6cm above the calcaneal attachment. Non-insertional tendinopathy is most frequently seen in the 30-50y.o. age group and is thought to affect between 7-9% of runners, but can also be seen in more sedentary individuals.
Treatment of Achilles’ tendinopathy also involves assessment of body mechanics and contributing physical factors, such as strength deficits and range of motion/flexibility deficits. However, rather than the “RICE” principle used in acute inflammatory conditions, research has shown a much more favorable response to increased loading of the tendon, specifically with eccentric, or “negative” type exercise. Eccentric loading, such as that experienced during the lowering phase of a standing heel raise exercise, has been shown to help stimulate new collagen tissue lay down in the damaged tendon, resulting in improved load-bearing capacity. Eccentric exercise may also affect the blood supply of the tendon, resulting in decreased pain.
The positive effects of eccentric exercise are most apparent in non-insertional tendinopathy, with mixed research results being shown in the treatment of those with insertional tendinopathy. Also of important note is the longer time-frame associated tissue remodeling, with most benefits of tendinopathy treatment occurring in programs of at least 12 weeks duration.
Whether you have recently suffered a complete tear of the Achilles’, or are dealing with a longer-standing, more chronic condition affecting your ability to work and play, consultation with a physical therapist can help determine an effective treatment approach to get you back on the road to pain-free function.

