Written by Nick Lacey on July 29, 2019 |
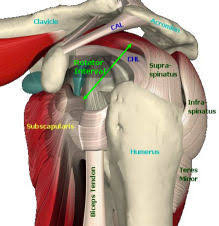
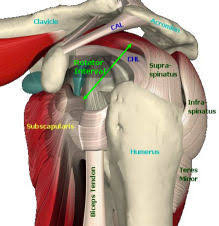
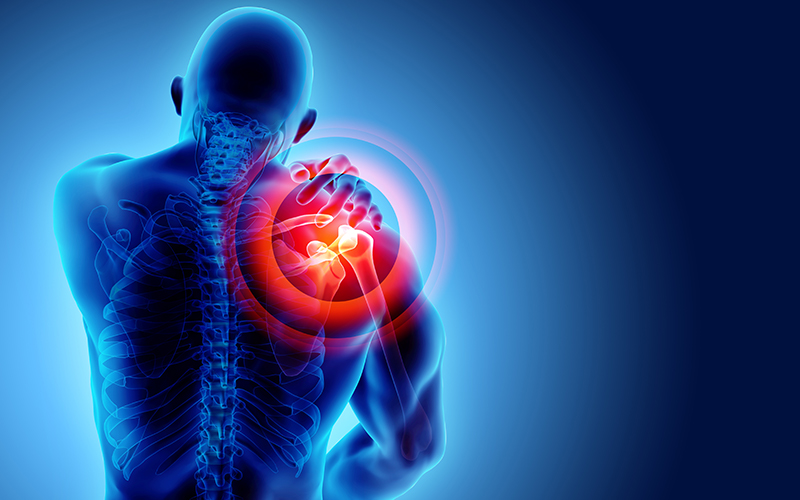
The rotator cuff interval (RI) is a critical area of the shoulder composed mostly of ligamentous tissue, as well as the long head of the biceps tendon. This area helps to stabilize the shoulder in the glenoid socket against forces that push the shoulder posteriorly or pull the shoulder down inferiorly. Common injuries that limit movements, such as shoulder impingement, rotator cuff muscle damage, and frozen shoulder may also involve the rotator cuff interval.
Continue Reading »
Written by Nick Lacey on July 24, 2019 |

What we know
- Repetitive concussions may have serious consequences over a lifetime
- Consecutive concussions prior to resolution of previous concussion may have detrimental long-term effects
- Called Secondary Impact Syndrome
- Most Concussions do not involve loss of consciousness
- Many concussions go unreported, increasing the risk of repeated traumas
- Youth injuries (5-14) are most often sports/bicycle accidents
- Children and adults experience the same post-concussive symptoms (DeMatteo, 2015)
Symptoms-Headache (71%), Distractible (57%), Memory Dysfunction, Dizziness (55%), Fogginess (53%), Sensitivity to light, Fatigue (50%), Blurred vision.
Youth Legislation
- H.R. 469 (2011) protects student athletes from concussions.
- Each state required to develop a standard plan for concussion safety
- All states have sports concussion laws as of 2014
Return to Play Protocol-Zurich Method
- Student athlete needs to return to the classroom first!
- One stage per day minimum without recurrence of symptoms
Stage 1-Cognitive rest-No TV, texting, computer. Resting stage until symptoms are free (at least 1 week.)
Stage 2-Stationary bike, TM (10-15 mins), low level activity
Stage 3-Mod exertion, more running drills. Sport specific activity.
Stage 4-At least 30 mins continuously, more cognitive load. Weight training.
Stage 5-Allowed contact in practice for the first time.
Stage 6-Has to be cleared by the physician before returning to game activity.
Current Multiple-Concussion Return to Play Guidelines
- Positive neuroimaging for 2 or more concussions= 3 months off contact sport
- 2 concussions in 3 months= 6 months off contact sport (From latest injury)
- 3+ concussions in 1 year=1 year off sport and retirement consideration
References
- www.Vestibular.org
- https://www.congress.gov/bill/112th-congress/house-bill/469
- Field, M, Collins, MW, Lovell, MR, Maroon, J. Does age play a role in recovery from sports-related concussion? A comparison of high school and collegiate athletes. J Pediatric. 2003;142:546-553.
- Toledo, E, Lebel, A, Bercerra, L. The young brain and concussion: imaging as a biomarker for diagnosis and prognosis. Neurosci Behav Rev. 2012;36:1510-1531
- DeMatteo, Carol et al. Development of a Conservative Protocol to Return Children and Youth to Activity Following Concussive Injury. Clinical Pediatrics. 2015 54(2) 152-163.
- Leddy J et al. A Preliminary Study of Sub symptomatic Threshold Exercise Training for Refractory Post-Concussion Syndrome. Clinical J of Sport Med 2010
- Burke, C. Stony Brook Neuro Concussion Assessment, 2017
Written by Tim Lewis on June 27, 2019 |
When it comes to shoulders, it is widely acknowledged that the glenohumeral joint (the GHJ, the shoulder joint that occurs due to the upper arm bone “attaching” to the body) has the most range of motion in the body. This joint can externally and internally rotate (as with reaching behind the head or reaching behind the back), flex and extend (as with reaching in front or behind), and adduct and abduct (as with reaching across the body or reaching out away from the body). In order to achieve such mobility, the shoulder blade must also move to allow the glenohumeral joint to be positioned appropriately.
Continue Reading »
Written by Tim Lewis on June 24, 2019 |
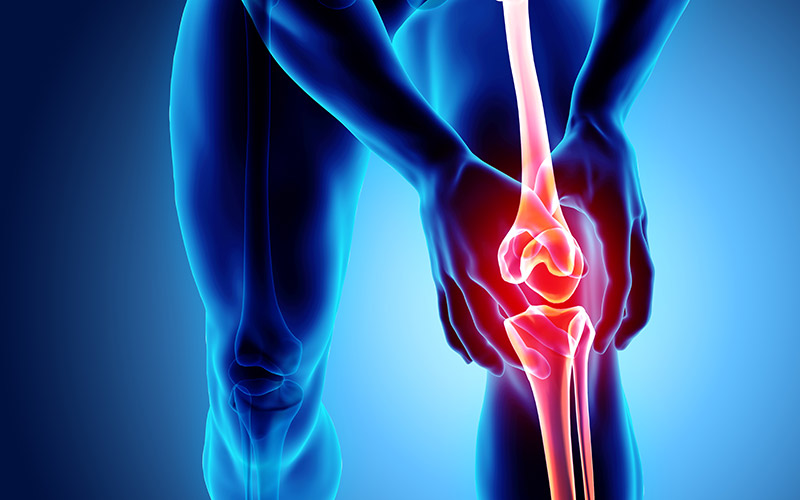
Now if you’ve ever heard of injuries to the knee, you have undoubtedly heard a bit about the dreaded “ACL Tear”. ACL tears (a tear of the Anterior Cruciate Ligament) tend to be a major cause of loss of functionality in people who injure this ligament. What people typically don’t realize is that the PCL (Posterior Cruciate Ligament) is another ligament of the knee that can be injured, albeit at a much less frequent rate.
Continue Reading »
Written by Emily on May 28, 2019 |

Spraining your wrist entails injuring the ligamentous structures surrounding the joint. The TFCC is one of the supporters of the wrist, supporting the hand and connection of the two forearm bones, radius and ulna. The TFCC stands for triangular fibrocartilage complex. In literature the TFCC is termed the “meniscus of the wrist,” because it functions similarly to the meniscus in the knee, distributing the load and partially absorbing the load in the wrist.
Continue Reading »
Written by Emily on May 21, 2019 |
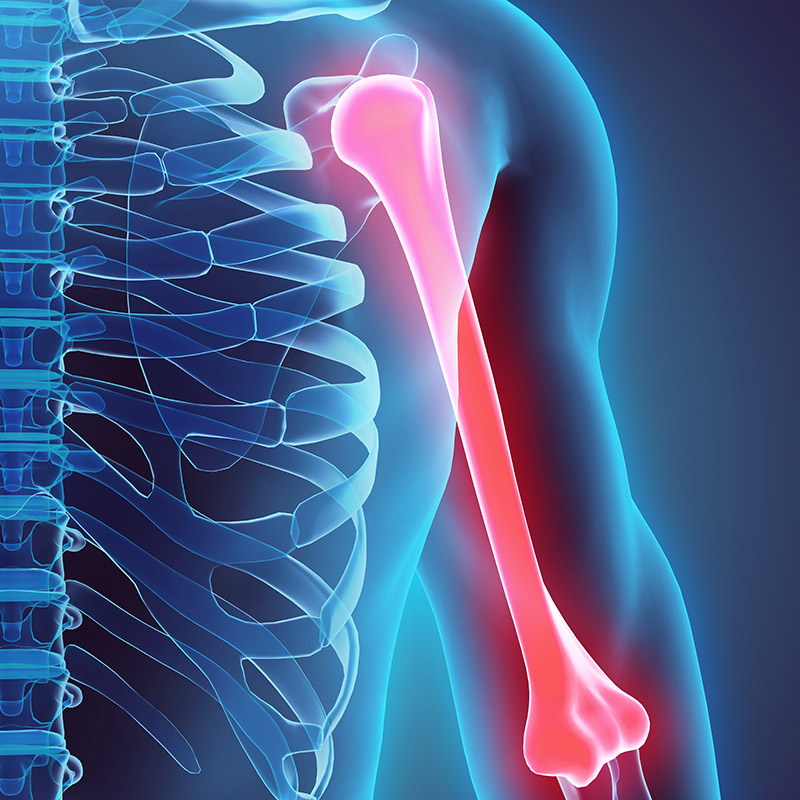
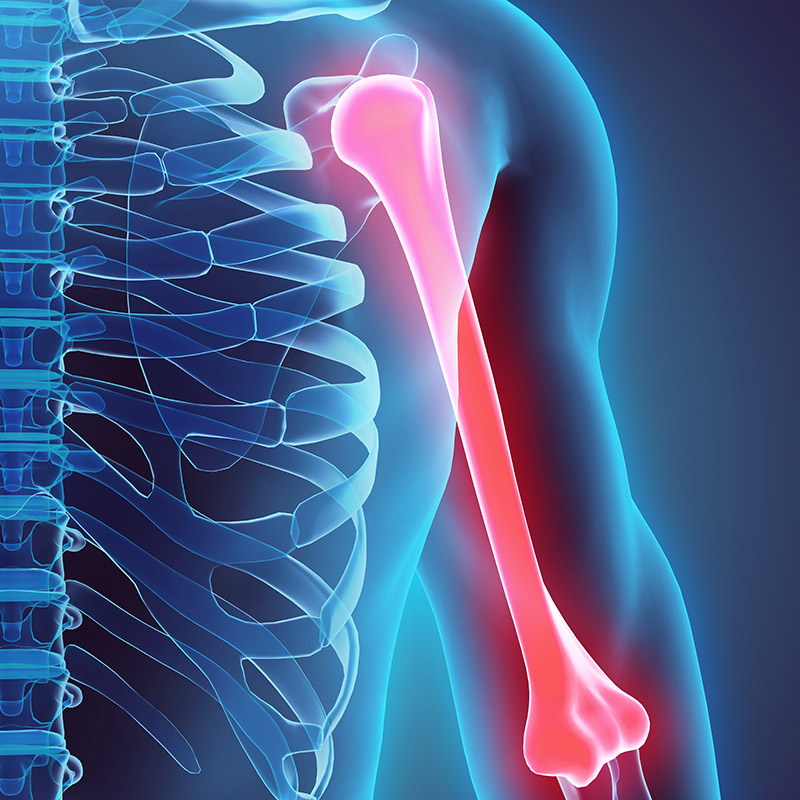
The humerus is the long bone of your upper arm. There are many muscles, ligaments, and nerves found along the humerus. Humerus fractures are named based upon the location of their fracture. Fractures which occur close to shoulder joint, injuring the ball and socket are proximal humerus fractures. Fractures which occur to the middle portion are called mid-shaft fractures and those along the lower portion are distal humerus fractures. With proximal humerus fractures, the majority are treated with a sling for 2-3 weeks and then exercises to regain function of the arm. More severe injuries of the proximal humerus may require surgical measures.
Continue Reading »
Written by Chelsea on April 24, 2019 |
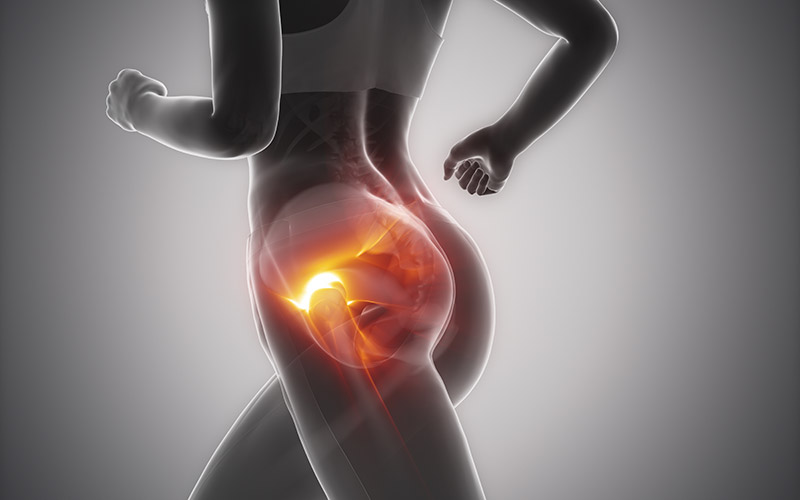
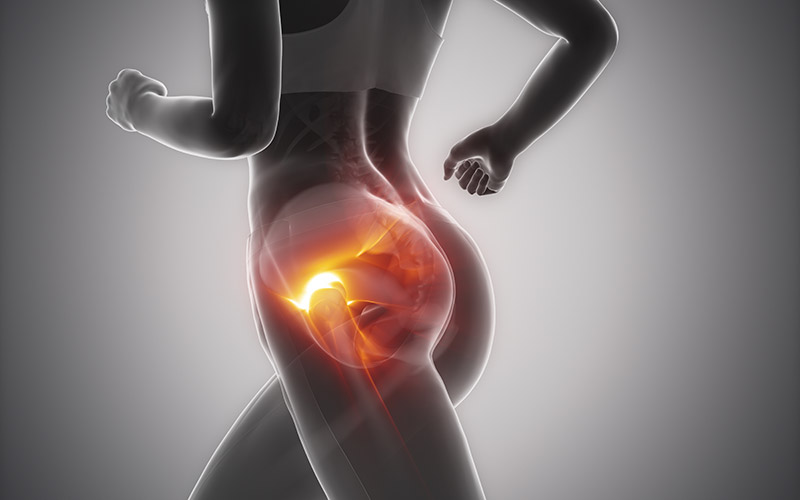
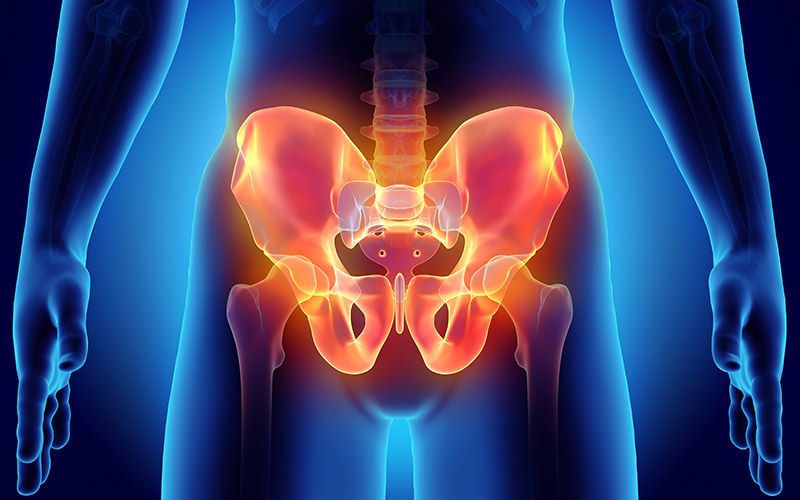
Hip pain is one of the more frequent complaints as people age, and many times it may be attributed to bursitis in the hip. Bursae are fluid-filled sacs that helps provide cushion between bone and soft tissue, and they can be found all over the body. When a bursa gets irritated or inflamed, it is referred to as bursitis. On the outside of the hip/upper thigh, there is a large bony point called the greater trochanter, and the trochanteric bursa is one of the more commonly affected areas where bursitis can occur (often referred to as trochanteric bursitis). Trochanteric bursitis can occur for a variety of reasons, including direct injury to the area, prior hip surgery, biomechanical factors like leg length differences or gait abnormalities, and overuse from repetitive activities like running, cycling, stair climbing, etc. Symptoms may include pain on the outer part of the hip that may or may not refer down the outside of the thigh or buttock, pain when lying on the affected side, pain getting in/out of the car or a deep chair, and pain with repetitive activities like walking, running, biking.
Conservative treatments like rest from overuse, ice, and NSAIDS may be effective to reduce inflammation and pain from trochanteric bursitis. Your doctor may also decide an injection may be beneficial to help relieve symptoms. Physical therapy can be very useful in helping reduce symptoms and prevent future exacerbations of pain as well. Exercises and manual interventions in physical therapy will aim to improve flexibility and mobility in surrounding areas that are tight, as well as improve strength in muscles that are weak, to improve the stabilization of the core, hips, and legs. Balance and proprioceptive exercises may also be given to help improve pelvic stability to aide with returning to your prior level of function.
If you have questions or would like more information on trochanteric bursitis, please contact us at ProActive Physical Therapy and Sports Medicine.
Reference:
Foran, Jared R.H. Hip Bursitis. https://orthoinfo.aaos.org . Reviewed September 2018. Accessed January 27, 2019.
Written by Chelsea on April 10, 2019 |

One of the most common dysfunctions to occur in the ankle/foot amongst both athletes and non-athletes is called posterior tibial tendonitis. The tibialis posterior is a muscle that starts from the back of the tibia (or shin bone). The tendon then runs down the inside of the leg and ankle, attaching on the inside of the foot near your arch. This tendon plays a crucial role in providing stability to the foot/ankle and supporting the arch of the foot with weight-bearing activities. Injury to the posterior tibial tendon can occur from trauma, like a fall. However, very commonly, overuse injuries occur from repetitive activities like walking, running, and jumping, causing pain and inflammation in the tendon. Classic symptoms of posterior tibial tendonitis include pain along the medial aspect of the ankle/foot, swelling, decreased range of motion, and sometimes instability in the foot/ankle. Because of the vital role the posterior tibial tendon plays in providing arch support, as the tendonitis progresses, the arch in the foot may flatten, changing the position of your foot and causing stress and strain in other areas of your ankle and foot as well.
Depending on the severity of dysfunction to the tendon, conservative treatment can be very successful in decreasing symptoms of posterior tibial tendonitis. This may include a regiment of rest, ice, compression, and possibly NSAIDS. Physical therapy can also be very beneficial to help improve range of motion, flexibility, and stability in the foot/ankle. Exercises to help stabilize the core and hip/pelvis may also be useful to improve overall mechanics of foot and ankle and prevent future injuries. In addition, orthotics may help to provide better arch support to decrease symptoms and prevent future injury as well.
If you have any questions about posterior tibial tendonitis or would like additional information, please contact us at ProActive Physical Therapy and Sports Medicine.
Reference
Weatherford, Brian M. Posterior Tibial Tendon Dysfunction. http://orthoinfo.aaos.org. Reviewed September 2017. Accessed January 26, 2019.
Written by Reyna Bucknell on April 4, 2019 |
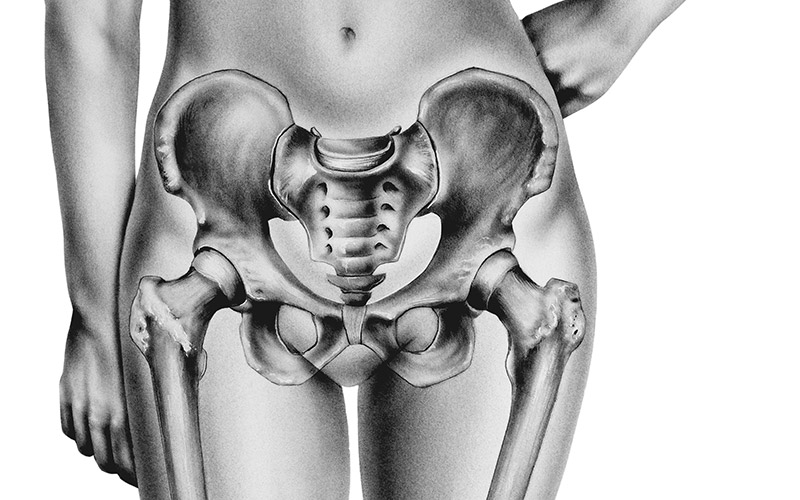
We often think that urine leakage is a normal part of aging. However, we have muscles in our pelvis called the pelvic floor muscles that are responsible for controlling this function and preventing urine from coming out at inappropriate times. Just like you would exercise your legs to keep walking and your arms to be able to carry your groceries, you should be exercising your pelvic floor muscles to stay in control of your bladder.
Continue Reading »
Written by Reyna Bucknell on March 7, 2019 |
Many women suffer from pelvic, vaginal, abdominal or rectal pain. They often undergo many tests and even invasive surgeries to try and fix this problem, but continue to suffer from pain. Many women are afraid to even approach the subject with their physicians because they are ashamed or embarrassed. Pain in these regions is not normal and it will likely not go away on its own. Pain is usually a sign of an underlying problem that needs to be addressed.
Continue Reading »