Frequently, individuals experience shoulder pain without any specific cause or trauma. As most people think, the smart thing to do in this situation would be to stop using the shoulder – avoiding any movement that would cause further pain. In the case of frozen shoulder, or adhesive capsulitis – conventional wisdom in this case is not so wise!
What is Frozen Shoulder?
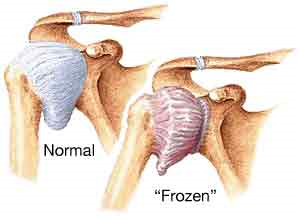
Frozen shoulder is a condition in which the soft tissue around the shoulder, or glenohumeral joint, becomes adhered and restricts normal shoulder mobility – especially the ability to turn the arm outward (external rotation), or reach behind the back (internal rotation) or overhead (flexion). Frozen shoulder predominantly occurs in individuals between the age of 40 and 65, more commonly in females than males. Frozen shoulder is also more common in those with hypothyroid conditions or diabetes. A hallmark sign of frozen shoulder is the onset of pain at the shoulder in the absence of significant trauma. Individuals may report having been more active with overhead activity, such as cleaning cabinets, or perhaps a very mild trauma, such as bumping the shoulder into a doorjamb or solid object.
Frozen shoulder can be defined as occurring in three different stages or phases – 1) “painful” or “freezing”, in which the predominant characteristic is shoulder pain, more so than stiffness, 2) “frozen”, where significant restricted shoulder mobility and pain are both present, and 3) “thawing”, where relatively little pain is noted, but major restrictions in shoulder joint mobility are prevalent. The typical time frame of frozen shoulder, from onset to resolution, may be anywhere from 1 to 2 years. Those affected by frozen shoulder often reclaim full shoulder mobility, but some individuals do continue to report mild to moderate limitations in shoulder range of motion (ROM) and function.
What can be done about Frozen Shoulder?
Early diagnosis of frozen shoulder is critical in minimizing the severity and duration of symptoms and limited function. For those falling in the higher risk categories (females, 40-65 years of age), putting off seeing a health care provider and receiving appropriate early treatment can result in a protracted period of pain and loss of function. Treatment in the early stages of adhesive capsulitis (“painful” or “freezing” phase) may include a corticosteroid injection by a physician, to help reduce inflammation of the shoulder tissues, resulting in decreased pain and potential stiffening of the shoulder tissues. Consultation with a physical therapist, who will evaluate the condition, prescribe appropriate exercises, and perform manual therapy techniques, is critical in speeding up the recovery from frozen shoulder. Exercises such as shoulder pendulums and wand exercises, emphasizing relative pain-free motion of the shoulder, have been shown to improve motion and upper extremity function. Manual therapy techniques, including shoulder joint mobilization, can help to maintain and improve mobility of the shoulder joint capsule and surrounding tissues, resulting in increased shoulder motion. Finally, education is paramount in treatment – patients need to know that movement of the involved arm is not only allowed, but encouraged, to prevent further stiffening of the shoulder.
If you feel that you may be experiencing symptoms of frozen shoulder, act quickly by contacting a healthcare provider, including a licensed physical therapist, to receive an accurate diagnosis and treatment. In this case, the phrase “move it or lose it” definitely applies!

