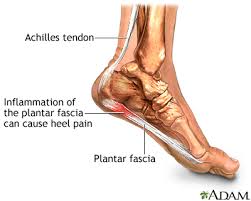
 Most people have heard of plantar fasciitis and know that it is a fairly common affliction of the foot. But many fewer individuals know what plantar fasciitis is (and how in the world “fasciitis” is actually pronounced!). Plantar fasciitis (“fash-ee-itis”) is a condition that affects the plantar fascia, a band of dense connective tissue (“fascia”) located at the bottom, or “plantar” surface of the foot, typically at the area of the heel bone (calcaneus). One of the most common foot problems addressed by health care professionals, plantar fasciitis is thought to affect upwards of 2 million Americans per year, and is estimated to affect one in ten individuals during their lifetime.
Most people have heard of plantar fasciitis and know that it is a fairly common affliction of the foot. But many fewer individuals know what plantar fasciitis is (and how in the world “fasciitis” is actually pronounced!). Plantar fasciitis (“fash-ee-itis”) is a condition that affects the plantar fascia, a band of dense connective tissue (“fascia”) located at the bottom, or “plantar” surface of the foot, typically at the area of the heel bone (calcaneus). One of the most common foot problems addressed by health care professionals, plantar fasciitis is thought to affect upwards of 2 million Americans per year, and is estimated to affect one in ten individuals during their lifetime.
Controversy exists in the very nature of plantar fasciitis, and whether it is truly an inflammatory condition (“-itis”) or not. Recent research suggests that in many cases when analyzed, the tissue affected exhibits an absence of specific chemical substances that define an acute inflammatory process. Hence, some researchers have begun to use the terms “plantar heel pain” or “plantar fasciopathy” to more accurately describe this condition. Although some doubt exists as to the nature of the condition, there is no doubt that plantar heel pain can create significant loss of function and negatively affect quality of life!
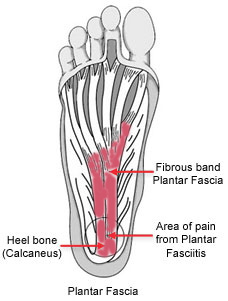 Plantar heel pain characteristically is experienced as pain at the bottom of the foot, within a few centimeters of the bottom of the heel. Symptoms include pain with initial weight bearing, typically noted during the first several steps after rising from bed in the morning, or after rising from sitting for prolonged periods. Pain generally eases after being up for several minutes to an hour, but will generally worsen as the day progresses, especially if remaining on the feet for prolonged periods during the day. Documented risk factors for plantar heel pain include limited ankle mobility (especially dorsiflexion, the ability to bring the foot upward) and higher body-mass index (BMI) in non-active individuals. Other risk factors associated with plantar heel pain includeprolonged time on the feet (occupational or recreational), and potentially affects those with non-neutral foot mechanics (excessively low or high arch) more frequently.
Plantar heel pain characteristically is experienced as pain at the bottom of the foot, within a few centimeters of the bottom of the heel. Symptoms include pain with initial weight bearing, typically noted during the first several steps after rising from bed in the morning, or after rising from sitting for prolonged periods. Pain generally eases after being up for several minutes to an hour, but will generally worsen as the day progresses, especially if remaining on the feet for prolonged periods during the day. Documented risk factors for plantar heel pain include limited ankle mobility (especially dorsiflexion, the ability to bring the foot upward) and higher body-mass index (BMI) in non-active individuals. Other risk factors associated with plantar heel pain includeprolonged time on the feet (occupational or recreational), and potentially affects those with non-neutral foot mechanics (excessively low or high arch) more frequently.
Recent studies have looked to determine which treatment options are effective in providing short and long-term benefit for those with plantar heel pain. Encouraging evidence has shown that exercise, specifically stretching of the major calf muscles and the plantar foot tissue, results in decreased pain. Stretches that have shown to be beneficial include the standing calf stretch, performed with hands placed against a wall and the affected leg placed behind the body with the foot flat on the ground. This stretch is best performed with the back knee held first in a straight, or locked out position, then again with the back knee bent. Performing this stretch with the knee straight, as well as bent, allows the gastrocnemius and the soleus, the primary muscles of the posterior calf, to both be stretched. The plantar fascia can be effectively stretched in a sitting position, with the affected foot resting crossed over on the opposite knee and the bottom of the toes grasped and pulled upward toward the shin of the same leg. Stretches can be held for various durations, but total stretch time for each exercise should be approximately three to five minutes, at least two times per day.
Another recent study has demonstrated that manual therapy provided by physical therapists, in conjunction with exercise, to be more effective than exercise alone. With physical therapists targeting specific tender spots (“trigger points”) in the soft tissue of the lower leg with hands-on techniques, patients have demonstrated significant short-term relief in plantar heel pain. Physical therapists can also perform techniques to address limited ankle mobility, as well as provide assessment of biomechanical factors, such as excessively flat feet (both identified as risk factors in plantar heel pain).
If you are experiencing the symptoms of plantar heel pain, consider seeing a physical therapist experienced in the treatment of musculoskeletal conditions, to help get you back on your feet again (without pain!).

